What My Doctor Missed
A Medical Mystery Solved While Building HealthScout
In my last post, My Next Learning Curve: Democratizing Healthcare, I made the case that patients need tools to put themselves on even footing with the complex and fragmented healthcare industry, and AI could be the catalyst to enable it.
Today I'm thrilled to announce HealthScout, a specially tuned AI chatbot designed to do just that — empower patients with their own health data coupled with the power of AI. Armed with HealthScout, patients can use their entire health record as context — across providers and time — to answer questions and explore options about their unique health journey. This is something people just can’t do using Google and generic AI chatbots.
True Story
While developing the app, I got to use it with my own health data, and was shocked that this combination of my health data plus AI revealed aspects of my health that neither my doctors nor I were aware of.
Patient (me):
Is there anything I can do about my worsening knee, back, and shoulder pain? Ibuprofen helps…but only for a few hours.Primary Care Physician:
I’ve had many patients successfully use over-the-counter doses of naproxen (Aleve) with great results. Take one in the morning and one at night for three days and see how you feel.
Later…
Patient (me):
It's been a bit over three weeks and I have to say, [naproxen has] made a significant improvement to all my joint problems. I'm actually able to do things I wasn't able to just a month ago. Good news, thank you!Questions: Am I on this forever now? Are there long term side effects?
Primary Care Physician:
I would say, take it for as long as you feel that you are getting benefit from it, and stop it periodically/regularly to see if you still need to be taking it. Many people take naproxen twice per day for decades.
So, I happily continued to take naproxen and later switched to a similar non-steroidal anti-inflammatory (NSAID) called celecoxib that clinical trials have shown to be easier on the stomach. I told friends of the miracle as well.
What My Doctor Saw
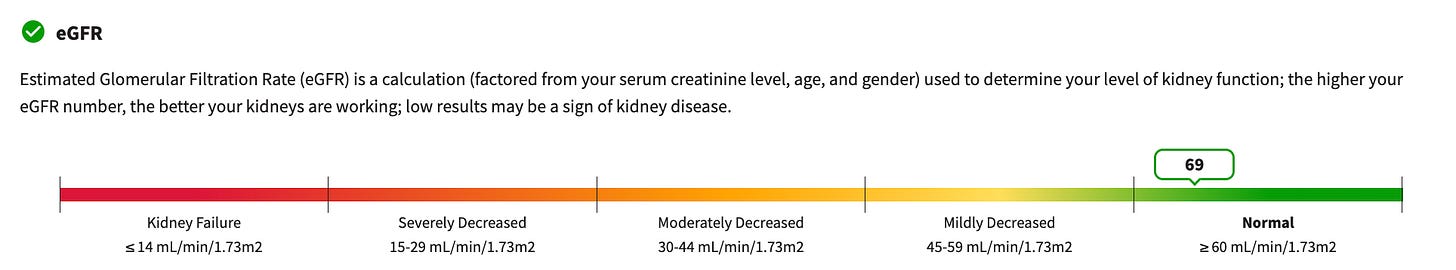
A year later at my next wellness check-up, my eGFR lab (a measure of kidney function) came back and looked like this.
On the lower end of Normal, is normal, right? My primary healthcare provider is One Medical, which allows doctors to spend a generous 30 minutes for wellness checks (many providers only allow 15 minutes). Still 30 minutes really isn’t that much time, so I’m guessing my doctor scanned my labs for “High” markers, and given the Labcorp generated chart above for my eGFR, he moved right past it.
I did too.
What HealthScout Saw
Four months later, when I started working on HealthScout, my own health records were the only data I could test with. As soon as it was hobbling, I excitedly started asking test questions of this fresh new AI model. One of my early questions to evaluate HealthScout’s analytical ability was:
Do you see any trends that show a relationship between my medications and my lab results?
To my surprise, HealthScout suggested that my recent kidney function decline could have something to do with my regular use of NSAIDs.
What???? What kidney function decline?!
I peppered HealthScout with lots of questions and learned exactly what it meant. Later I built this chart showing what HealthScout saw (HealthScout doesn’t have charting…yet).
Unlike my One Medical primary care physician, HealthScout had access to my entire health history across three providers over a decade.
With this historical context, HealthScout saw that my eGFR steady state was around 90, and when it dropped 30% in only seven months, that’s at least a yellow flag.
Further, while it seems many primary care physicians use the standard > 60 eGFR as “normal” measure as shown in the Labcorp chart, HealthScout knew about a more granular classification nephrologists (kidney doctors) use. Under this kidney health classification system, my 69 eGFR was not really “normal,” but rather quickly approaching “moderate” kidney disease as shown in the chart above.
Last, HealthScout recognized that I started on my NSAIDs in February 2024. It connected the dots and suggested that my NSAID use could have caused my kidney function to decline.
Wow.
What Are The Implications
Of course, HealthScout’s observation about my kidney health being related to NSAID use is correlation and not causation. It noted that many other factors could have caused my eGFR to be lower including being poorly hydrated on the day of the test, complications with other medications, eating too much protein, and sadly “age.”
I’m not confident HealthScout (or anyone) could answer definitively why my eGFR went down, but HealthScout was the first system to point out that it did go down in a concerning way.
This experience highlights how HealthScout can help:
Identify patterns in your health data that individual doctors might miss
Connect information across multiple healthcare providers and years of records
Translate concerning trends into actionable questions for your next doctor visit
Put you in control of your complete health story
Because of HealthScout, I'm now armed with intelligent questions for my doctor about my kidney health. That's the essence of how HealthScout can empower you.
Update September 17, 2025.
PostScript
After I wrote this original post, my kidney function worsened, I was referred to a nephrologist (kidney specialist), and ended up getting a biopsy, which confirmed that NSAIDs caused my kidney function decline.
The good news is that as long as I stay off NSAIDs, drink lots of water, and eat a healthy diet, my kidneys should heal.
HealthScout Now Available!
Even better news — the beta is over and HealthScout is now available. If you’re curious if your own health records contain hidden information, download HealthScout free from the App Store.






Doctors relying solely on today's AI for diagnosis is like writers relying solely on spell checkers for spelling errors. Of course, both AI and spell checkers are wrong some of the time.
But they both are both hugely valuable! That said, both also require responsible use. Double-check your work!
Just yesterday, to a very sad story about medical misdiagnosis, I posted a warning about the risks of future doctors relying on AI to make their diagnostic decisions. This offers a patient-AI model but it’s an N=1 case example.
As a health researcher and critic of clinical trials but no defender of the medical profession, I’d be wary of over generalization. It would be good if those who take you up on your suggestion form a group to share their experiences both positive and negative.